As many people contemplate waiting for a shoulder replacement and they have the time to review the research, they see that they have three main options to manage their shoulder pain and shoulder injuries.
Replace the ball and socket of the shoulder joint. The reason a shoulder replacement can be tricky is that the joint is more a golf ball and tee than a ball and a socket like the hip. This, as we will see from the research, can make shoulder replacement a technically challenging surgery.
Manage the shoulder with “conservative non-surgical treatments,” such as painkillers, anti-inflammatories, cortisone, physical therapy, and other remedies for as long as you can until the pain or loss of function becomes unbearable.
Try regenerative medicine such as stem cell therapy and platelet rich plasma therapy.
This article will feature different treatments including surgery, PRP, and stem cells.
If you went to the doctor with shoulder pain, and you had a shoulder MRI, and that MRI revealed shoulder osteoarthritis, the next discussion you will probably have with your doctor is what can you do about it? That answer is not clear cut. What treatments you take can be influenced by the amount of pain and function that you have.
A physical examination should also include screening for physical abnormalities—swelling, deformity, muscle weakness, and tender areas—and observing the range of shoulder motion—how far and in which directions the arm can be moved. Although x rays may be helpful in defining problems, more elusive ones may require computerized tomography (CT scan), which provides a more detailed view of the bones. Electrodiagnostic studies such as the electromyogram (EMG) and a nerve conduction study can indicate whether pain or weakness in the area is coming from a pinched nerve in the neck, or a peripheral nerve injury away from the neck, or down the arm. Magnetic Resonance Imaging (MRI) and ultrasound are other safe and effective diagnostic tools, providing images of the soft tissues without using radiation. An arthrogram is an x ray, CT or MRI in which dye is injected into the joint for added contrast. However, as outlined in other sections of this website, studies have shown that the advanced technologies commonly used to diagnosis injuries are grievously insufficient to show where the pain is coming from.
Treatment options for shoulder or glenohumeral osteoarthritis
This February 2022 paper (1) examined the treatment options for older patients with shoulder or glenohumeral osteoarthritis and provides the basis of treatment. Many of the people who come to us for other treatments options have already followed and unfortunately failed many of these interventions.
Here are the learning points of this research:
Glenohumeral osteoarthritis (arthritis of the ball and socket of the shoulder) is a common cause of shoulder pain and is characterized by articular cartilage thinning, glenoid bone loss and deformity, osteophytosis (bone spurs), and other associated changes. . . Non-pharmacological treatment options may serve as adjuvants to other therapies and should be incorporated for a more holistic approach to management. Pharmacological treatments include oral agents such as acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, corticosteroids and antidepressants.
Intra-articular injections such as platelet-rich plasma, cortisone, and hyaluronic acid are usually used to control symptoms in moderate to advanced arthritis or in non-surgical candidates. Other non-surgical treatment options include suprascapular nerve block and radiofrequency ablation, and these options have been studied on different levels of evidence. Surgical treatment of Glenohumeral osteoarthritis is reserved for patients who do not respond to conservative management or who suffer from debilitating symptoms that severely impair their quality of life.
Conservative treatment is this a realistic plan to get pain-free range of motion?
When someone comes into our institute it is usually after the “conservative treatments,” have failed their shoulder injuries and damage and that a surgery is being strongly recommended. What people, perhaps one day like yourself, who come into our office want is a realistic plan to get them to a pain-free range of motion in a functioning shoulder. Many times we can get people to this goal, many times we come close to getting people to this goal with significant improvement to their quality of life. There are times when we can only help a little. There are times we cannot help at all. People we cannot help would be significantly advanced cases of degenerative shoulder disease. Perhaps 10 to 20% of patients who seek regenerative medicine will not be good candidates. This is why I invite people to email me to discuss before they make an appointment. You can do so as well by using the form below.
A January 2023 paper (x) found that a structured home exercise program (HEP) and active, supervised physiotherapy (PT) after primary Reverse Total Shoulder Arthroplasty demonstrated similar results in improving function and range of motion following total reverse shoulder replacement. Suggesting that it may not be necessary to recommend PT as a protocol for all patients after total reverse shoulder replacement.
The realistic outcome some patients can expect is that when they agree to the shoulder replacement surgery, they have to be prepared for the likely outcome of the necessity for multi-surgeries.
We do a lot of research in our clinic, one topic we research often is shoulder osteoarthritis. There are many new studies on the problems of shoulder replacement and fixing a failed replacement.
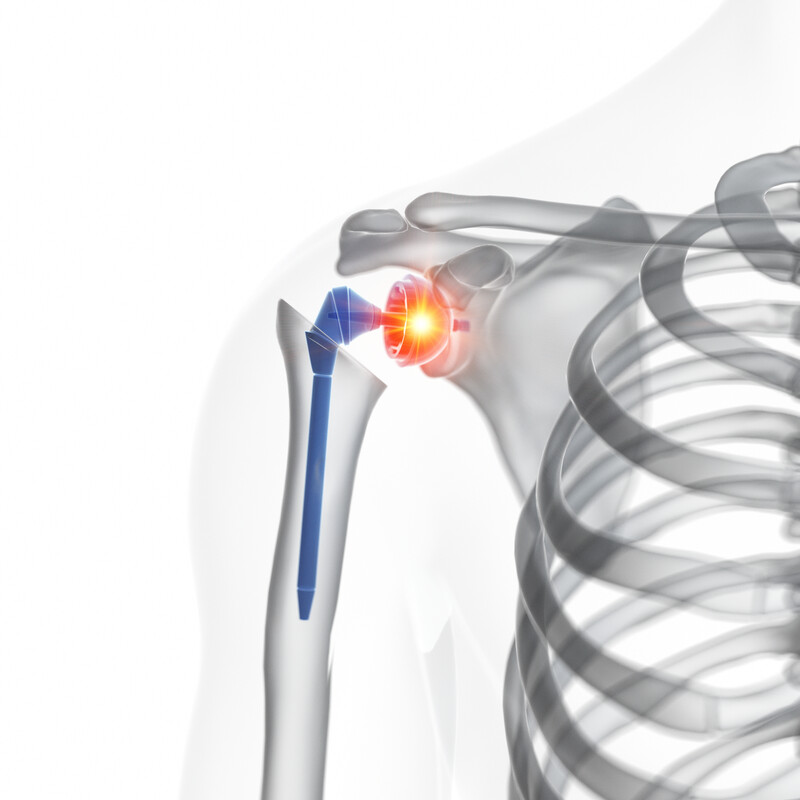
Here is a recent study from a Swedish research team. It appears in the journal Acta orthopaedica (2) and discusses shoulder hemiarthroplasty. Shoulder hemiarthroplasty is a procedure where the ball of the shoulder is replaced with a prosthetic, while the socket (or tee) remains intact.
The two types of Shoulder hemiarthroplasty are:
- shoulder resurfacing hemiarthroplasty (a protective metal cap is placed over the ball of the humerus head)
- shoulder stemmed hemiarthroplasty (imagine a thumb tack, the metal cap is attached to a metal stem which is pushed into the humerus head)
Shoulder hemiarthroplasty comes with a high risk of need for second surgery. To quote the research: “. . . while patients receiving resurfacing hemi and stemmed hemi, reported similar shoulder functionality and quality of life, the revision rate for resurfacing hemi (12%) . . . stemmed hemi (6.7%).
The purpose of this study was to find why there was such a difference.: The results were:
- The younger patients were more likely to receive the resurfacing shoulder hemiarthroplasty and since younger people live longer, the chances of need or more revision surgery is greater. So a skewed result is achieved resurfacing shoulder hemiarthroplasty have a higher risk for revision because the patients were young enough to have multiple surgeries.
- The older you were, the more likely you would get the shoulder stemmed hemiarthroplasty because you suffered from primary osteoarthritis. Then you had a 6.7% chance of going back to surgery. Since the patients were older, as we have seen in other studies, they would be less likely to want to undergo a second or revision surgery. Older adults fearful of revision surgery also can skew results.
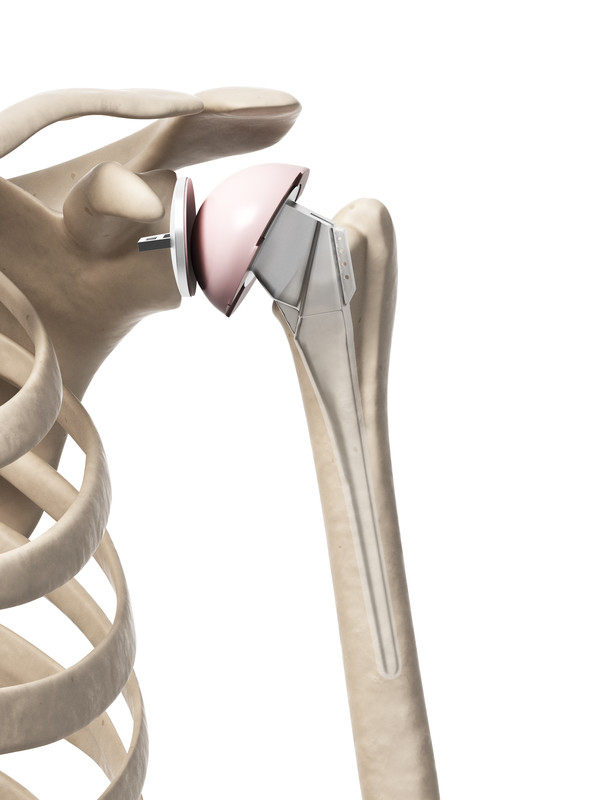
Reverse total shoulder arthroplasty replacement vs standard total shoulder replacement
An August 2022 paper (18) compared Reverse total shoulder arthroplasty replacement with standard total shoulder arthroplasty (replacement). These are the findings: “Reverse total shoulder arthroplasty (Reverse total shoulder arthroplasty replacement), which was originally designed mainly for irreparable rotator cuff damage, has gained popularity in recent years for the treatment of advanced shoulder osteoarthritis instead of the clinically standard total shoulder arthroplasty (replacement). However, this Reverse total shoulder arthroplasty has some nonnegligible flaws such as higher complications rate and economic cost, not mention the following problems caused by irreversible physical structural damage. Therefore, the employment of Reverse total shoulder arthroplasty needs to be carefully considered.”
In this study of 57,156 shoulder arthroplasties, “Reverse total shoulder arthroplasty patients in the rotator cuff deficiency group had significant higher transfusion rates and longer hospital stays. Reverse total shoulder arthroplasty patients without rotator cuff deficiency had a statistically significantly higher number of implant-related mechanical complications, acute upper respiratory infections and postoperative pain. Overall, Reverse total shoulder arthroplasty incurred higher costs in both groups. For osteoarthritis patients with rotator cuff deficiencies, Reverse total shoulder arthroplasty has its benefits as complication rates were comparable to total shoulder arthroplasty. For those patients without rotator cuff deficiencies, the use of Reverse total shoulder arthroplasty should be reconsidered as there were more complications with higher severity.”
People have failed shoulder surgeries and doctors cannot pinpoint why
A 2022 paper (17) citing the above research says this: “We found worse outcomes for patients with previous surgery for instability independent of age, sex, and arthroplasty (resurfacing the bones or joint replacement) type. The reason cannot be deduced from our study and there is no adequate explanation in the literature. Several factors could, in theory, have an adverse effect on the outcome for these patients. A long history of instability and previous surgery may lead to eccentric glenoid wear and subsequently a technically demanding operation with risk of persisting instability, subluxation of the humeral component, or loosening of the glenoid component.”
What was the outcome of the necessity for revision shoulder replacement surgery in this study group?
An August 2021 study (14) assessed the rate of complications associated with the need to recommend patients to a revision shoulder arthroplasty.
Patients were recommended to a revision shoulder replacement surgery because of:
- component loosening 20% (601 patients of 3,041 patients in the study)
- shoulder instability 19% (577 patients of 3,041 patients),
- rotator cuff failure 17% (528 patients of 3,041 patients),
- and infection 16% (490 patients of 3,041 patients).
Many people have rotator cuff repair prior to shoulder replacement. The hope of course is that arthroscopic rotator cuff will improve rotator cuff problems and repair rotator cuff defect. In these surgeries rotator cuff healing may not occur and then the patients will develop rotator cuff disease.
Revision complications
- Intraoperative complication (complication during the revision surgery) was 8% (230 of 2,915 patients in the study)
- Postoperative complication was 22% (825 of 3,843 patients in the study), and
- Reoperation rates were 13% (584 of 3,843 patients in the study).
For various reasons some chose not to have the secondary surgery. The authors concluded: “Satisfactory improvement in patient-reported outcome measures are reported following revision shoulder arthroplasty; however, revision surgery is associated with high complication rates and better outcomes may be evident following revision to reverse shoulder replacement.”
You have had a successful surgery but still have severe shoulder pain. How? Researchers tried to gauge what constituted the minimum results necessary to call a shoulder replacement surgery a success.
In the Journal of shoulder and elbow surgery, researchers tried to gauge what constituted the minimum results necessary to call a shoulder replacement surgery a success. In 326 patients who had either a total shoulder replacement, a primary reverse shoulder replacement, or hemiarthroplasty, in averaging out the patient response outcomes, the researchers found that patients treated with a shoulder arthroplasty require a 1.4-point improvement in the visual analogue pain score (2) (a scoring system of 0- no pain and 10 extreme pain), most of you reading this article will be very aware of this pain scoring system and how it works).
- If you went to surgery with, for an example 8.4 VAS score or very severe pain, you qualified for a minimal clinically important difference (success) if you reported that pain down to a 7.0. The successful surgery still left you in severe pain. Any pain relief is welcome, but how many people would have the surgery for a 10% improvement?
Why patients fail to achieve the minimal acceptable results to consider the surgery successful?
A November 2021 study (15) compared patient-reported outcomes (PROs) and range of motion (ROM) measurements between patients achieving and failing to achieve a Patient Acceptable Symptom State (PASS) after anatomic total shoulder arthroplasty (replacement) to determine which patient-reported outcomes (PROs) questions and range of motion (ROM) measurements were the primary drivers of poor outcomes.
In this study 301 patients who had undergone primary total shoulder replacement at least two years prior. The primary outcome was the difference in active range of motion (ROM) between patients achieving and failing to achieve the Patient Acceptable Symptom State (minimum requirement) threshold for the American Shoulder and Elbow Surgeons (ASES) and Single Assessment Numeric Evaluation (SANE) scores. The secondary outcome was the difference in self-reported pain levels between those achieving and failing to achieve the minimum requirement.
- Based on the American Shoulder and Elbow Surgeons Patient Acceptable Symptom State threshold, 87% (261/301) of patients achieved a minimally successful total shoulder replacement, whereas 13% did not.
- Based on the Single Assessment Numeric Evaluation Patient Acceptable Symptom State threshold, 69% (208/301) of patients achieved a achieved a minimally successful total shoulder replacement, whereas 31% did not.
- Patients who failed were younger and had lower short form-12 mental health scores than those who did.
- There was a significant difference in pain between those who achieved and failed to achieve a minimally successful total shoulder replacement.
- Those failing had significantly higher pain levels and worse function.
Conclusion: There is variability in the percentage of patients who achieve a a minimally successful total shoulder replacement, ranging from 69% to 87% depending on the patient-reported outcome scoring systems used to define the threshold. Patients who did not achieve a minimally successful total shoulder replacement were significantly more likely to have pain, whereas there were very few differences in range of motion, indicating pain as the primary driver of failing to achieve a successful surgery.
How strong is your shoulder after shoulder replacement? “While some patients saw improvement in function, surgeon (and patient) should be aware that durability and strength of rotation would be weak.”
Beyond pain, there is the question of function, strength and durability of the replaced shoulder. There is a lot of research focusing on a patient’s ability to resume normal activity or return to their favorite sport after shoulder replacement. Many studies suggest a great deal of success in the shoulder replacement. Other studies are less favorable.
A study from November 2019 (3) compared the isometric strength and endurance of shoulder abduction and internal and external rotation between operated shoulders and non-operated shoulders in the same patient. The patient underwent reverse shoulder replacement due to degenerative rotator cuff tear.
Who was in this study?
- 41 consecutive patients (average age of about 71 years old; 36 females vs 5 males) who underwent reverse shoulder replacement. All 41 patients had no symptoms in the other shoulder and normal shoulder function.
- The average length of follow-up was 34 months.
Results
- Patients exhibited improvement in functional level in the replacement shoulder.
- The limitations however following surgery were In the strength and endurance of internal and external rotation which were lower in operated shoulders than the patient’s other shoulder. The durability of internal and external rotation were significantly lower in operated shoulders.
- While some patients saw improvement in function, surgeon (and patient) should be aware that durability and strength of rotation would be weak.
“There is currently no consensus on recommended levels of activity and sport following reverse total shoulder arthroplasty.”
From July 2019 and the journal Shoulder & Elbow.(4)
- “Reverse total shoulder arthroplasty is now the most frequently performed form of shoulder replacement. There is currently no consensus on recommended levels of activity and sport following Reverse total shoulder arthroplasty.”
- “Return to sport is tolerated following Reverse total shoulder arthroplasty; however, studies are short to medium term only and although the reported complication rate is low, the studies did not include radiographic evaluation. Longer term studies with subgroup analysis evaluating common recreational activities after Reverse total shoulder arthroplasty are required, particularly in the younger population, in order to establish clear post-operative guidelines.”
When shoulder replacement has a higher risk for failure and causes shoulder pain
The above statement is not an opinion, it is in the research:
- In a paper published in the March 2017 issue of the Journal of Shoulder and Elbow Surgery, doctors in Germany evaluated and identified risk factors for the development of intraoperative and postoperative surgical complications in total shoulder arthroplasty in patients with primary osteoarthritis. Twenty-seven complications (9.8%) in 275 shoulder arthroplasties were recorded. Mostly from patients who practiced poor lifestyle choices.(5)
- Also appearing in the Journal of Shoulder and Elbow Surgery, February 2017 issue, doctors at the Steadman Hawkins Clinic of the Carolinas wrote that patients’ resilience, that is the ability to bounce back or recover from stress, an increasingly recognized psychometric property, would do better than patients who do not do well with stress. The patients with low resilience would suffer from greater shoulder complications.(6)
- Doctors at the University Medical Center of Cologne in Germany also published new research in which a bad problem is can be made much worse by shoulder replacement. The German doctors suggest that a preoperative evaluation of humeral head subluxation (the head of the shoulder is not where it is supposed to be) and glenoid erosion (the shoulder labrum has deteriorated), two factors associated with less favorable postoperative shoulder replacement results, should be considered before moving forward to surgery.(7)
Poor lifestyle choices and failed shoulder replacement
These are just a few of the studies which if you read them as a whole tells us that patients with poor lifestyle choices, those who do not bounce back well from adversity, those whose shoulders have significant degeneration of the soft tissue, should be offered an alternative to shoulder replacement.
Here is a report from doctors at the Mayo Clinic. It was published in the Journal of shoulder and elbow surgery (8) December 18, 2017 edition. Here are the highlights:
- 42 patients who had shoulder replacement, two patients had both shoulders replaced. Minimum 10 year follow up. Goal: Long-term assessment of shoulder replacement
- Studies have demonstrated mixed results after humeral head replacement for osteoarthritis at short- and medium-term follow-up intervals.
- Some patients experienced significant pain relief postoperatively that was maintained during the long-term follow-up
- 11 patients more than 25% of the study group reported persistent moderate or severe pain minimum ten years out
- Ten of 44 (22.7%) shoulders underwent revision surgery, predominantly for glenoid arthrosis (arthritis) (n = 9).
- In the 25 shoulders with 5 years of radiographic follow-up, patients demonstrated moderate to severe glenoid erosion in 50% at 5 years, which increased to 59% at 15 years and 88% at 20 years.
Humeral head replacement remains a successful operation for osteoarthritis at long-term follow-up. However, there is a substantive subgroup with continuing pain and a high rate of glenoid bone erosion after 10 years. Surgeons should carefully consider patients’ needs and desires when judging the indications for humeral head replacement.
Despite research showing increasing numbers of surgical failures, more patients are having shoulder replacement surgery.
The above study shows the concern for the high number of complications measured long-term in shoulder replacement patients. In a study published in the journal Radiographics, radiologists (9) looked for key imaging features in patient shoulders to help them distinguish between the shoulder problems listed above. If they could find MRI evidence for the source of pain, radiologists could guide surgeons in choosing the type of replacement surgery the patients should get. This they suggested would help limit surgical failures and get the shoulder to as normal a range of motion as possible.
Sounds good, but as we have seen in patients here in our clinic that had an MRI, had the source of their pain pinpointed, had preoperative planning, had the best prosthetic device for them, had the best intention of the health providers to get that shoulder to as good as new as possible. The surgery still failed catastrophically.
In a study in the Journal of Elbow and Shoulder Surgery, doctors put a great degree of surgical failure on the shoulder instability the surgery itself caused.
Here is the researchers report:
- 27 patient case studies were reviewed. These patients had experienced shoulder replacement postoperative instability
- The type of surgeries were 8 hemiarthroplasties (ball replacement and structural fix of the bone),
- 14 total shoulder replacements with metal-backed glenoid components, and
- 5 total shoulder replacements with cemented glenoid components.
The patients had:
- 10 isolated subscapularis tears,
- 6 massive rotator cuff tears,
- 8 component malpositions,
- 2 component dissociations or loosening, and
- 1 humeral shortening. (10)
As pointed out above, stress from surgery can put a lot of pressure on a rotator cuff tendon. This can cause component loosening.
One thing certainly that would help prevent surgical failure is not having a surgery.
In the Mayo clinic study above, bone disintegration was a great concern. In a recent study, also in the Journal of shoulder and elbow surgery, doctors discuss hardware failures known to plague patients: “The longevity of total shoulder replacement is primarily limited by the performance of the ultra high-molecular-weight polyethylene glenoid component. [This study] demonstrates that glenoid component fracture associated with oxidation has not been eliminated with the advent of modern materials (HXL) in the shoulder domain.”
In other words, the hardware caused an oxidation problem which disintegrated the bone.(11)
The health of bone is obviously very important in shoulder replacement. As you can imagine a revision surgery to fix the problems created by bone disintegration caused by the first replacement will be a complex one.
The following research also from the Journal of Shoulder and Elbow Surgery explains why patients must be given information on treatment options outside of surgery:
- “The management of a failed shoulder represents a complex and difficult problem for the treating surgeon, with potential difficulties and complications that are related to the need to remove a well-fixed stem.”(12)
If the prosthesis is removed due to failure, the bone becomes compromised, and it is even more difficult to place another prosthesis.
The search for shoulder replacement alternatives – is Stem cell therapy for shoulder pain a realistic treatment option?
The problem with shoulder replacement failures are leading researchers to look at shoulder replacement alternatives including stem cells . One study found that surgical repairs of degenerate and torn tissue are often prone to failure, and that some biological (biomedical) therapies (such as Platelet-Rich Plasma Therapy or Stem Cell Therapy) might improve outcomes. In fact, injections of platelet-rich plasma have led to reduced pain and improved recovery in other degenerated areas, together with the restoration of function. More research on stem cells is also forthcoming.
The stem cell therapy treatment procedure is seen in this video
The stem cell procedure uses adult stem cells or mesenchymal stem cells.
Doctors in Germany looked at repairing cartilage defects and soft tissue injury (typically rotator cuff injuries and tearing) in the shoulder before it leads to advanced osteoarthritis. They concluded that Stem Cell Therapy for cartilage regeneration was a minimally invasive approach for shoulder joint preservation and an alternative to shoulder replacement.(11)
In the video below, I demonstrate of technique for giving PRP Injections into the shoulder
- Notice that multiple areas of the shoulder are treated in this stem cell procedure / treatment.
- The stem cells injected in this procedure is well tolerated by this patient.
Can PRP therapy and stem cell treatments be an option for shoulder pain?
In the worst case of shoulder replacement I have seen, an elderly man presented with right shoulder pain. When I asked him to lift his arms, he lifted his right arm, but had no motion at all in his left shoulder. I was perplexed and asked if his left shoulder also hurt. His response was alarming. He told me he had a left shoulder replacement, and the arm prosthesis had dislocated out the the shoulder, and he had absolutely no use of his left arm since the dislocation that could not be relocated into the false joint. He obviously wanted to avoid surgery to his right shoulder.
We also see people who already had many surgeries and now so little is left of their shoulder they have to have a shoulder replacement. I myself had arthroscopic shoulder surgery many years ago. It did not help me and it took a year of rehab just to get it back to what it felt like just before the surgery. I see this in people all the time. They have a shoulder surgery, they rehab for a year, the shoulder still hurts, they have another shoulder surgery, they rehab for one year then it is deiced that they have reached the point of no return, shoulder replacement, they only decision left is reverse shoulder replacement or a shoulder replacement. So now that this person is waiting to get a shoulder replacement, what happens next? For some, cortisone injections to hold them over. Cortisone injections, as it has been demonstrated, can accelerate avascular necrosis or bone death. So a person has had two surgeries and they may have no cartilage left, now they are getting cortisone, now they will have no bone left.
When people reach out to our office asking about stem cell therapy in fixing their bad shoulder we tell them stem cell therapy will help many people in varying degrees of success. Stem cell therapy however will usually not be able to help the person who has no range of motion in their shoulder or it is fused or frozen in place by bone spurs. There has to be a realistic expectation of what stem cells can do.
“The application of different growth factors and mesenchymal stem cells appears as promising approaches for enhancing biologic repair”
A study (13) in the The open orthopaedics journal from 2017 wrote: “The application of different growth factors and mesenchymal stem cells appears as promising approaches for enhancing biologic repair. However, data from clinical studies are still limited, and future studies need to improve understanding of the repair process in cellular and molecular level and evaluate the effectiveness of biologic factors in the management of shoulder disorders.”
The Darrow Stem Cell Institute has published research on the treatment of shoulder osteoarthritis and rotator cuff tears with bone marrow derived stem cells. The research appears in the peer-reviewed journal Cogent Medicine. The study can be found here in its entirety: Treatment of shoulder osteoarthritis and rotator cuff tears with bone marrow concentrate and whole bone marrow injections with a June 20, 2019 publication date.
An extended summary can be found here on our website: Treatment of shoulder osteoarthritis and rotator cuff tears.
The learning points of this research are as follows:
- Patients who received either one and two treatments of bone marrow derived stem cells reported significant improvements in resting pain, active pain, and functionality score when compared to baseline.
- These groups also experienced a 42.25% (one treatment) and 50.17% (two treatments) overall improvement respectively after receiving the stem cells.
- The group that received two treatments experienced statistically significant improvements in active pain when compared to the group that received one injection.
- There were no significant outcome differences between rotator cuff tear and osteoarthritis patients.
Conclusions: Our study demonstrated that patients diagnosed with shoulder osteoarthritis or rotator cuff tears experienced symptomatic improvements in pain and functionality when injected with bone marrow concentrate (BMC) stem cells or whole bone marrow (WBM) stem cells. Further randomized control studies are needed to validate these findings.
More information on these treatments can be found in my articles on the stem cell procedure and rotator cuff injuries:
- Rotator cuff tears – Stem cell therapy, PRP, cortisone and surgery
- Shoulder Labrum tear | Labral repair and biceps tenodesis
The use of bone marrow concentrate (BMC) stem cells or whole bone marrow (WBM) stem cells and the realistic outcomes that stem cell treatments can have for you should be discussed after a physical examination. In some patients stem cells can offer a good outcome and in some patients stem cells may not be a realistic option. For many people this depends on the range of motion in the shoulder, whether bone spurs have developed, the extent of injury and damage to the rotator cuff muscles, if previous surgery repaired rotator cuff tendons and ligaments.
Stem cells as a treatment can help many people. To assess your candidacy for treatment to possibly help avoid shoulder replacement please email using the form below.
Do you have questions about shoulder stem cell or stem cell procedures? Ask Dr. Darrow

11645 WILSHIRE BOULEVARD SUITE 120, LOS ANGELES, CA 90025
PHONE: (800) 300-9300 or 310-231-7000
References
1 Al-Mohrej OA, Prada C, Leroux T, Shanthanna H, Khan M. Pharmacological Treatment in the Management of Glenohumeral Osteoarthritis. Drugs & Aging. 2022 Feb;39(2):119-28.
2 Ödquist M, Hallberg K, Rahme H, Salomonsson B, Rosso A. Lower age increases the risk of revision for stemmed and resurfacing shoulder hemi arthroplasty: A study from the Swedish shoulder arthroplasty register. Acta orthopaedica. 2017 Dec 5:1-7.
2 Tashjian RZ, Hung M, Keener JD, Bowen RC, McAllister J, Chen W, Ebersole G, Granger EK, Chamberlain AM. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. Journal of shoulder and elbow surgery. 2017 Jan 1;26(1):144-8.
3 Erşen A, Birişik F, Bayram S, Şahinkaya T, Demirel M, Atalar AC, Demirhan M. Isokinetic Evaluation of Shoulder Strength and Endurance after Reverse Shoulder Arthroplasty: A Comparative Study. Acta Orthop Traumatol Turc. 2019 Nov;53(6):452-456. doi: 10.1016/j.aott.2019.08.001. Epub 2019 Aug 19. PMID: 31439480; PMCID: PMC6939012.
4 MacInnes SJ, Mackie KE, Titchener A, Gibbons R, Wang AW. Activity following reverse total shoulder arthroplasty: What should surgeons be advising?. Shoulder & elbow. 2019 Jul;11(2_suppl):4-15.
5 Leschinger T, Raiss P, Loew M, Zeifang F. Total shoulder arthroplasty: risk factors for intraoperative and postoperative complications in patients with primary arthritis. J Shoulder Elbow Surg. 2017 Mar;26(3):e71-e77. doi: 10.1016/j.jse.2016.08.001. Epub 2016 Oct 10.
6 Tokish JM, Kissenberth MJ, Tolan SJ2, et al. Resilience correlates with outcomes after total shoulder arthroplasty. J Shoulder Elbow Surg. 2017 Feb 10. pii: S1058-2746(17)30012-5. doi: 10.1016/j.jse.2016.12.070.
7 Leschinger T, Raiss P, Loew M, Zeifang F. Predictors of medium-term clinical outcomes after total shoulder arthroplasty. Arch Orthop Trauma Surg. 2017 Feb;137(2):187-193. doi: 10.1007/s00402-016-2602-x. Epub 2016 Dec 7.
8 Robinson WA, Wagner ER, Cofield R, Sanchez-Sotelo J, Sperling JW. Long-term outcomes of humeral head replacement for the treatment of osteoarthritis; a report of 44 arthroplasties with minimum 10-year follow-up. Journal of shoulder and elbow surgery. 2017 Dec 18.
9 Lin DJ, Wong TT, Kazam JK. Shoulder Arthroplasty, from indications to complications: what the radiologist needs to know. Radiographics. 2016 Jan-Feb;36(1):192-208. doi: 10.1148/rg.2016150055.
10 Kany J, Jose J, Katz D, Werthel JD, Sekaran P, Amaravathi RS, Valenti P. The main cause of instability after unconstrained shoulder prosthesis is soft tissue deficiency. Journal of Shoulder and Elbow Surgery. 2017 Feb 27.
11 Ansari F, Lee T, Malito L, Martin A, Gunther SB, Harmsen S, Norris TR, Ries M, Van Citters D, Pruitt L. Analysis of severely fractured glenoid components: clinical consequences of biomechanics, design, and materials selection on implant performance. J Shoulder Elbow Surg. 2016 Jan 14. pii: S1058-2746(15)00588-1. doi: 10.1016/j.jse.2015.10.017
12 Giotis D, Aryaei A, Vasilakakos T, Paschos NK. Effectiveness of Biologic Factors in Shoulder Disorders. Open Orthop J. 2017;11:163–182. Published 2017 Feb 28. doi:10.2174/1874325001711010163
13 Cisneros LG, Atoun E, Abraham R, Tsvieli O, Bruguera J, Levy O. Revision shoulder arthroplasty: does the stem really matter? J. Shoulder Elbow Surg. 2016 Jan 25. pii: S1058-2746(15)00578-9. doi: 10.1016/j.jse.2015.10.007.
14 Ravi V, Murphy RJ, Moverley R, Derias M, Phadnis J. Outcome and complications following revision shoulder arthroplasty: a systematic review and meta-analysis. Bone & Joint Open. 2021 Aug 2;2(8):618-30.
15 Cole EW, Moulton SG, Werner BC, Denard PJ. Why patients fail to achieve a Patient Acceptable Symptom State (PASS) after total shoulder arthroplasty?. JSES international. 2022 Jan 1;6(1):49-55.
17 Rasmussen JV, Olsen BS. Previous surgery for instability is a risk factor for a worse patient-reported outcome after anatomical shoulder arthroplasty for osteoarthritis: a Danish nationwide cohort study of 3,743 arthroplasties. Acta Orthopaedica. 2022;93:588.
18 Liu H, Huang TC, Yu H, Wang Y, Wang D, Long Z. Total shoulder arthroplasty versus reverse total shoulder arthroplasty: Outcome comparison in osteoarthritis patients with or without concurrent rotator cuff deficiency. Medicine (Baltimore). 2022 Aug 12;101(32):e29896.
x Chalmers PN, Tashjian R, Keener J, Sefko JA, Da Silva A, Morrissey C, Presson AP, Zhang C, Chamberlain AM. Active Physical Therapy Does Not Improve Outcomes After Reverse Total Shoulder Arthroplasty: A Multi-Center, Randomized Clinical Trial. Journal of Shoulder and Elbow Surgery. 2023 Jan 21.
5125