What is microfracture knee surgery?
Knee microfracture surgery is a common arthroscopic procedure where an awl (a sharp pointed tool) is pushed into the bone where the protective knee cartilage has worn away. The small holes made by the awl are called microfractures. The goal of this surgery is to build new cartilage.
A multinational research team that includes the Harvard Medical School says evidence suggests that patient outcomes improve with microfracture for the most part, but in some studies these effects are not sustained. They highlight their study with these points:
- The quality of cartilage repair following microfracture is variable and inconsistent due to unknown reasons.
- Younger patients have better clinical outcomes and quality of cartilage repair than older patients.
- Patients with smaller lesions have better clinical improvement than patients with larger lesions.
- The necessity of long postoperative CPM (Continuous passive motion) and restricted weight bearing is widely accepted but not completely supported by solid data.
- All in all there is limited evidence that micro fracture should be accepted as gold standard for the treatment of cartilage lesions in the knee joint.(8)
This is not the only research to question the microfracture procedure’s effectiveness. Doctors at the Federal University of São Paulo in Brazil published their findings in which they compared microfracture to other surgical procedures. In their findings there was no evidence that allograft transplantation (cartilage transplantation from a donor) or microfracture drilling worked any better than each other. But they did note that “treatment failure, with recurrence of symptoms, occurred with both procedures.”(9)
Surgical Cartilage treatment strategies are characterized as:
- Chondroplasty, a procedure that shaves down or smooths out of cartilage.
- Debridement (power washing the the knee cartilage),
- Microfracture,
- Transplantation autologous chondrocyte implantation [ACI], osteochondral autograft [OAT], and osteochondral allograft [OCA]).
Authors from the University of New Mexico Health Sciences Center concluded: These techniques may improve patient outcomes, though no single technique can reproduce normal hyaline cartilage. (10)
In agreement are Ohio State University researchers who say: The markedly limited healing potential of articular cartilage often leads these patients to continued deterioration and progressive functional limitations even after surgery. (11)
The problem with surgery is that it cannot do what patients want most – repair and regrow damaged tissue.
Autologous chondrocyte transplantation
In an October 2022 study, (16) doctors examined postoperative complications and associated risk factors for failure following autologous chondrocyte transplantation as well as its long-term survival and clinical function. The doctors hypothesized that “autologous chondrocyte transplantation is a safe technique for cartilage repair with a low incidence of postoperative complications and rare rates of revision surgery combined with a high long-term survival and good to excellent clinical outcome in long-term-follow-up.” This is what they found:
- Postoperatively, 8% of patients had complications (4% bleeding, 2% arthrofibrosis, 2% infection)
- 7% of patients needed revision surgery.
- 12% of patients had a prolonged deficit in range of motion, that did not require revision surgery.
- Patients demonstrated good patient reported long-term outcomes 9-15 years after the surgery.
- Survival rates were 88% at 9 years, 85% at 11 years, and 85% at 13 years after the surgery.
The study indicates “autologous chondrocyte transplantation is an “effective treatment option for femorotibial- as well as patellofemoral cartilage defects with a high long-term survival and low conversion rate as well as good long-term results regarding knee function and satisfaction. Postoperative complications needing revision surgery are rare.”
Biological knee reconstruction without surgery – using stem cells
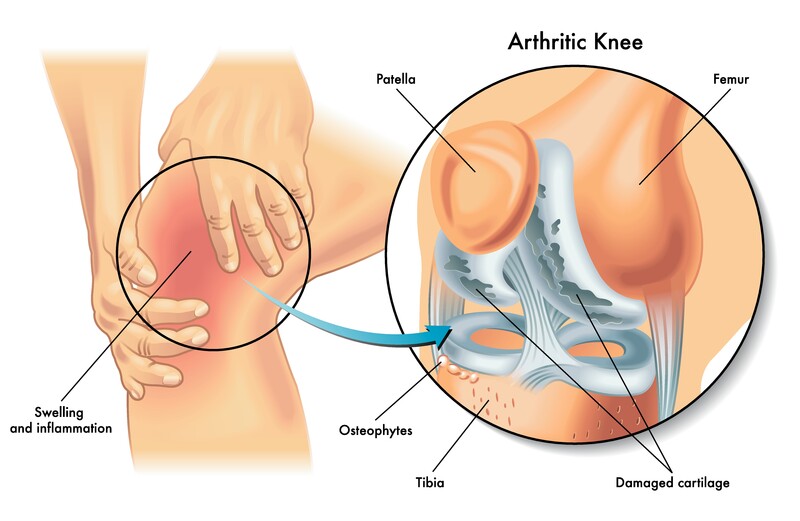
The definition of osteochondral is that it is related to the cartilage and bone. In the knee joint cartilage protects the shinbone, the thigh bone, and the back of the kneecap or the patella. A healthy knee has all its surfaces glide smoothly atop these cartilages for pain free, efficient, and in the case of athletics – explosive movement. In recent research investigators suggested that knee stem cell therapy could provide the answer where drug interventions and surgical procedures were lacking:
- “Drug interventions and surgical treatments have been widely attempted for cartilage regeneration in osteoarthritis. However, the results were largely unsatisfactory. Autologous chondrocyte implantation (ACI) or matrix-induced autologous chondrocyte implantation (MACI) offers potential for the regeneration of cartilage over the long-term. However, due to the limitations and disadvantages of ACI, alternative therapies for cartilage regeneration are in need. The availability of large quantities of mesenchymal stem cells (MSCs) and the multilineage differentiation (the morphing ability), especially their chondrogenic (for cartilage) differentiation property, have made MSCs the most promising cell source for cartilage regeneration.”(12)
From the medical journal Stem cell research & therapy “Since the cartilage is composed primarily of chondrocytes (a specialized cartilage cell) bone marrow-derived mesenchymal stem cells with its ability to morph into these cartilage cells appear to be ideally suited for therapeutic use in cartilage regeneration.” (13)
I have much more information on this site concerning stem cell therapy for knee osteoarthritis and degenerative knee disease. Please start here with this article on knee osteoarthritis and stem cell treatments. To learn more about stem cell therapy visit my stem cell therapy research page.
Do you have questions? Ask Dr. Darrow
A leading provider of stem cell therapy, platelet rich plasma and prolotherapy
11645 WILSHIRE BOULEVARD SUITE 120, LOS ANGELES, CA 90025
PHONE: (800) 300-9300 or 310-231-7000
References
1 Wang D, Gonzalez-Leon E, Rodeo SA, Athanasiou KA. Clinical Replacement Strategies for Meniscus Tissue Deficiency. Cartilage. 2021 Nov 20:19476035211060512. doi: 10.1177/19476035211060512. Epub ahead of print. PMID: 34802295.
2 Lee BS, Bin SI, Kim JM, Kim WK, Choi JW. Survivorship After Meniscal Allograft Transplantation According to Articular Cartilage Status. Am J Sports Med. 2017 Apr;45(5):1095-1101. doi: 10.1177/0363546516682235. Epub 2017 Jan 10.
3 Ogura T, Bryant T, Minas T. Biological Knee Reconstruction With Concomitant Autologous Chondrocyte Implantation and Meniscal Allograft Transplantation: Mid- to Long-term Outcomes. Orthopaedic Journal of Sports Medicine. 2016;4(10):2325967116668490. doi:10.1177/2325967116668490.
4 Wang D, Kalia V, Eliasberg CD, Wang T, Coxe FR, Pais MD, Rodeo SA, Williams III RJ. Osteochondral Allograft Transplantation of the Knee in Patients Aged 40 Years and Older. The American Journal of Sports Medicine. 2017 Nov 1:0363546517741465.
5 Antosh IJ, Cameron KL, Marsh NA, Posner MA, DeBerardino TM, Svoboda SJ, Owens BD. Likelihood of return to duty is low after meniscal allograft transplantation in an active-duty military population. A Publication of The Association of Bone and Joint Surgeons®| CORR®. 2020 Apr 1;478(4):722-30.
6 Searle H, Asopa V, Coleman S, McDermott I. The results of meniscal allograft transplantation surgery: what is success?. BMC musculoskeletal disorders. 2020 Dec;21(1):1-9.
7 Ahmed AF, Rinaldi J, Noorzad AS, Zikria BA. Return to Sports Following Meniscal Allograft Transplantation is Possible but Remains Questionable: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2021 Nov 14.
8 Erggelet C, Vavken P. Microfracture for the treatment of cartilage defects in the knee joint – A golden standard? J Clin Orthop Trauma. 2016 Jul-Sep;7(3):145-52. doi: 10.1016/j.jcot.2016.06.015.
9 Gracitelli GC, Moraes VY, Franciozi CE, Luzo MV, Belloti JC. Surgical interventions (microfracture, drilling, mosaicplasty, and allograft transplantation) for treating isolated cartilage defects of the knee in adults. Cochrane Database Syst Rev. 2016 Sep 3;9:CD010675.
10 Richter DL, Schenck RC Jr, Wascher DC, Treme G. Knee Articular Cartilage Repair and Restoration Techniques: A Review of the Literature. Sports Health. 2015 Oct 12. pii: 1941738115611350. [Epub ahead of print]
11 Campbell AB, Pineda M, Harris JD, Flanigan DC. Return to Sport After Articular Cartilage Repair in Athletes’ Knees: A Systematic Review. Arthroscopy. 2015 Oct 30. pii: S0749-8063(15)00706-9. doi: 10.1016/j.arthro.2015.08.028.
12 Qi Y, Yan W. Mesenchymal stem cell sheet encapsulated cartilage debris provides great potential for cartilage defects repair in osteoarthritis. Med Hypotheses. 2012 Sep;79(3):420-1. Epub 2012 Jun 1.
13 Zhang L, Hu J, Athanasiou KA. The Role of Tissue Engineering in Articular Cartilage Repair and Regeneration. Critical reviews in biomedical engineering. 2009;37(1-2):1-57.
14 Trivedi J, Betensky D, Desai S, Jayasuriya C. Post-traumatic osteoarthritis assessment in emerging and advanced pre-clinical meniscus repair strategies: A Review. Frontiers in Bioengineering and Biotechnology. 2021 Dec 22:1352.
15 Liu J, Bloom DA, Dai AZ, Mahure SA, McAllister D, Strauss EJ, Jazrawi LM, Campbell KA. The State of Meniscal Allograft Transplantation in New York Over the Last Decade. Bulletin of the Hospital for Joint Disease (2013). 2022 Sep 1;80(3):239-45.
16 Ehmann YJ, Esser T, Seyam A, Rupp MC, Mehl J, Siebenlist S, Imhoff AB, Minzlaff P. Low postoperative complication rate with high survival rate and good clinical outcome 9 years after autologous chondrocyte transplantation of the knee joint. Archives of Orthopaedic and Trauma Surgery. 2022 Oct 5:1-0.
2372