Many emails that come in from this website, come from people asking about SLAP tear surgery. Some people want to know if they can avoid surgery. Some people are looking for options because they cannot get a SLAP tear surgery. Why can’t they get the surgery? Because their doctor/surgeon does not hold out good hope that surgery will be effective for them. Who are these people? From the emails we get, they are usually people with multi-directional shoulder instability, or, people who already had the surgery and despite it being a successful surgery, the person still had pain and range of motion issues.
Before we get into the research, here is my story. I have a labral tear in my right shoulder. I have a supraspinatus and subscapularis tear as well. I also have NO pain. How do I know I have the tears? Because I looked at my shoulder under ultrasound when I was having shoulder pain, one day especially, when I had a frozen shoulder from hitting too many golf balls. I am a very repetitive motion type athlete.
I did have a shoulder surgery while I was in medical school. I had the orthopedic surgeon I was under perform it. The surgery was not successful. In fact, for me, it was terrible. The reason I got into this line of non-surgical medicine was because of the results I got in myself using regenerative medicine techniques. I have treated and healed my shoulder using Platelet Rich Plasma Therapy and Stem Cell Therapy. I’ve injected both my shoulders, both my knees, both my elbows, and wrist. This is not to say that this will work for everyone, but it worked for me.
The surgical decision for labral tear or SLAP tear
When faced with a diagnosis of labral tear or SLAP tear, younger athletes or athletic individuals will usually weigh treatment options based on getting back to sport, or for some, work the quickest. If surgery gets them back the fastest, then many will favor the surgery despite research that suggests outcomes may not be what was hoped for or expected. See the research below. For others a more conservative care approach is taken. Resting the shoulder, icing the shoulder, and taking anti-inflammatory medications are usually recommended. If the shoulder is not responding, physical therapy will next be recommended. If there is pain, a cortisone injection may be offered. When these conservative treatment fail, surgery will often be recommended.
What type of surgery?
- Older patients maybe recommended to biceps tenodesis: This procedure addresses biceps tendon tear or biceps tendonitis (inflammation of the tendon). In this surgery, those portions of the tendon are removed. In some cases the tendon has to be detached and reattached.
- Younger patients will get a Superior labrum, anterior and posterior (SLAP) surgery. These surgeries can include:
- Labrum debridement: In this surgery the frayed edges of the labrum are trimmed or “power washed” away. The goal is to reduce the risk of future tearing by trimming back the torn area of the labrum. Typically this is an arthroscopic procedure.
- Labrum repair. These surgeries can include:
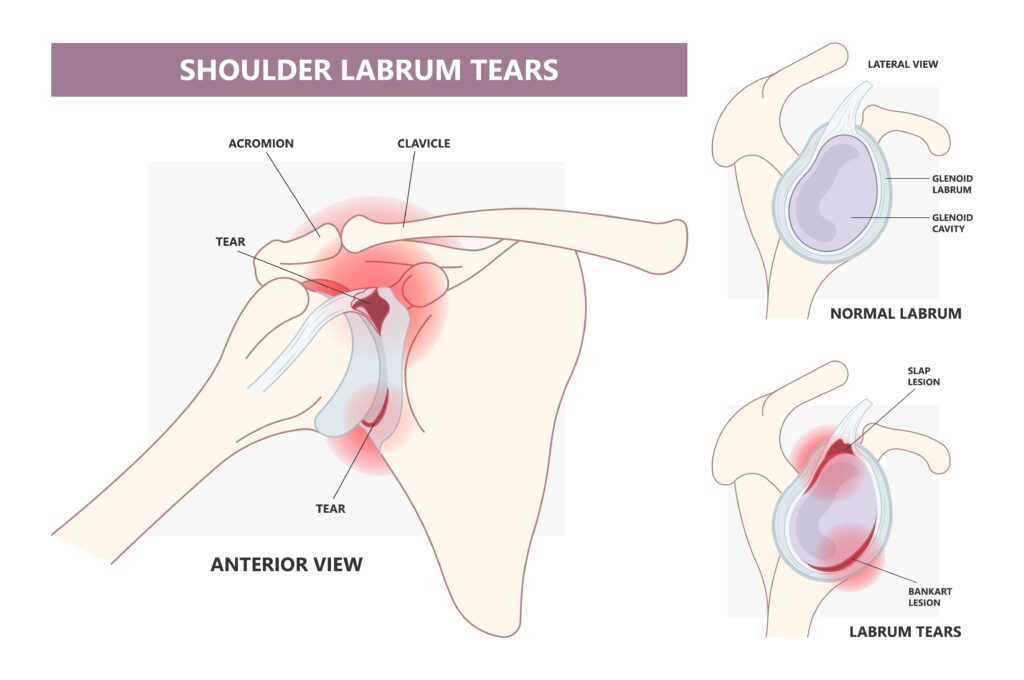
- SLAP (superior labrum from anterior to posterior) a front of the shoulder to back of the shoulder labrum tear. In a SLAP repair the damaged material of the tear is removed, then small holes are drilled into the bone so the remnant labrum can be sutured to the bone via anchors placed into the bone.
- A Bankart Repair is a surgical procedure that seeks to prevent future and chronic anterior shoulder dislocations due to instability in the back of the shoulder. In this surgery ligaments and the shoulder cartilage are repaired (if possible).
Returning to sport and work following surgery – “the most appropriate surgical option in elite throwers is controversial.”
There are many studies that assess the patient’s ability to return to sport and work following an arthroscopic shoulder procedure. A July 2021 study (14) provides this summary assessment of returning to sports and work after the procedures.
- Superior labrum, anterior and posterior (SLAP) lesions are common and identified in up to 26% of shoulder arthroscopies, with the greatest risk factor appearing to be overhead sporting activities.
- Symptomatic patients are treated with physical therapy and activity modification. However, after the failure of non-operative measures or when activity modification is precluded by athletic demands, SLAP tears have been managed with debridement, repair, biceps tenodesis or biceps tenotomy. Recently, there have been noticeable trends in the operative management of SLAP lesions with older patients receiving biceps tenodesis and younger patients undergoing SLAP repair, largely with suture anchors.
- For overhead athletes, particularly baseball players, SLAP lesions remain a difficult pathology to manage secondary to concomitant pathologies (other shoulder damage) and unpredictable rates of return to play.
- As a consequence, the most appropriate surgical option in elite throwers is controversial.
Research does not give clear evidence that athletes return to their previous level of sport or athletic performance following surgery
An October 2020 study (15) says: “Limited evidence suggests that less than three in four athletes return to their previous level of sport participation after SLAP injury intervention. Treatment success for an athlete with SLAP injury remains relatively unknown as only 59% of included studies clearly delineate RTS (return to sport) from RTSP (return to sport at previous level) and neither athletic performance nor career longevity were reported in any included studies.”
“Neither labral repair nor biceps tenodesis had any significant clinical benefit over sham surgery for patients with SLAP II lesions in the population studied.”
In May 2017, A Norwegian research team lead by Dr Cecilie Piene Schrøder, an Orthopedic surgeon, examined the effectiveness of the routine surgical procedures they were performing for SLAP lesions or tears of the shoulder. Here is what the research team noted:(1)
- Labral repair and biceps tenodesis are routine operations for superior labrum anterior posterior (SLAP) lesion of the shoulder, but evidence of their effectiveness is lacking.
- We (the research team) evaluated the effect of labral repair surgery, biceps tenodesis surgery and sham (placebo) surgery on SLAP lesions.
So what Dr. Schrøder and his colleagues were looking for was to see if the surgeries they were performing actually worked by comparing them to a Sham or placebo surgery.
- They did a a double-blind, sham-controlled trial with 118 surgical candidates (average age 40 years), with patient history, clinical symptoms and MRI arthrography indicating an isolated type II SLAP lesion.
- Forty patients were randomly assigned to get a labral repair surgery.
- Thirty-nine patients received a biceps tenodesis surgery.
- Thirty-nine patients received a sham surgery.
- Results There were no significant between-group differences at any follow-up in any outcome.
- Conclusion Neither labral repair nor biceps tenodesis had any significant clinical benefit over sham surgery for patients with SLAP II lesions in the population studied.
59.1% of patients returned to the same or higher level of play.
A March 2022 study (13) examined whether performing open subpectoral biceps tenodesis in overhead athletes with a superior labrum anterior to posterior (SLAP) tear may affect their ability to return to overhead sports. The current study included 44 overhead athletes. The average age was 34.9 years, 79.5% were male, and the average follow-up was 49.0 months.
- Overall, 81.8% of patients returned to play their overhead sport after biceps tenodesis, and
- 59.1% of patients returned to the same or higher level of play.
- It took patients, on average, 8.7 months to return to play after biceps tenodesis.
A November 2022 study (17) suggests “The surgical management of type II superior labrum anterior and posterior (SLAP) tears in patients younger than 40 years is controversial, but growing evidence suggests comparable outcomes between primary SLAP repair and primary biceps tenodesis, with lower rates of reoperations after primary biceps tenodesis.”
“Most SLAP lesion patients, however, are ultimately treated non-operatively.”
In July 2018, Dr. Schrøder followed up his paper with a short piece published in the The open orthopaedics journal. Here he addressed criticism about his findings. When questioned on the usefulness of SLAP tear surgery, Dr. Schrøder responded: “Based on (our) results we have narrowed our indications for SLAP lesion surgery. We still treat some SLAP lesions surgically and individualize our treatment in each such cases. Most SLAP lesion patients, however, are ultimately treated non-operatively.”(2)
Another 2018 study, this time from Department of Orthopaedic Surgery, Stanford University (3) found that “The management of Type-II superior labral tears (SLAP) of the shoulder remains a controversial topic. Treatment ranges from non-operative management to surgical management including SLAP repair, biceps tenotomy, and biceps tenodesis. An optimal treatment algorithm has yet to reach universal acceptance.”
These researchers suggested: “Management of Type-II SLAP tears remains a diagnostic and therapeutic challenge, especially in the context of lack of consensus in the literature. Surgical management includes labral repair, biceps tenodesis, biceps tenotomy, or a combination. Clinical decision making should be based on patient age, desired activity levels, the degree of participation in overhead sports, and the presence or absence of other associated pathology. These variables should be considered carefully as the surgeon and patient develop the ideal surgical treatment plan after conservative measures have failed.”
The Hospital of Special Surgery and the Mayo Clinic findings say mixed results
A January 2018 study from the Hospital of Special Surgery and the Mayo Clinic discussed the diagnostic and treatment challenges presented by injuries to the biceps and superior labral complex.
“Nonoperative management, even in overhead athletes, has demonstrated relatively good outcomes, while operative outcomes have yielded mixed results. The surgeon must take into account a number of variables when choosing the appropriate surgical procedure: labral repair versus biceps tenodesis. Rehabilitation, either as nonoperative management or as a postoperative protocol, should focus on restoring glenohumeral and scapulothoracic strength, endurance, and full, pain-free range of motion, while correcting any deficiencies in balance or rhythm throughout the overhead motion.”(4)
A bicep tenodesis is a surgery to repair a damaged bicep tendon. A biceps tenodesis may be performed as an isolated procedure but more often is part of a larger shoulder surgery, including rotator cuff repair.A recent study from Rush University Medical Center warns of including this procedure during the bigger shoulder surgery:
“High-demand patients with biceps tendonitis in the setting of a SLAP lesion with labral instability who undergo combined tenodesis and SLAP repair have significantly worse outcomes than patients who undergo either isolated labral repair for type II SLAP tears or isolated biceps tenodesis for a SLAP tear and biceps tendonitis.”(5)
It takes nine months to recover from surgery to return to sport – unless you are a throwing athlete or pitcher
A December 2019 paper (16) offered these timetables for a return to sport in evaluating individuals undergoing arthroscopic SLAP repair. This research encompasses 22 previously published articles involving a total of 944 patients undergoing arthroscopic SLAP repair.
- Of the total included patients, 270 were identified as overhead athletes, with 146 pitchers.
- Across all patients, 69.6% (657/944 patients) of individuals undergoing arthroscopic SLAP repair returned to sport.
- There was a 69.0% (562/815 patients) return to previous level of play, with a mean time to return to sport of about nine months.
- The return-to-sport rate for pitchers compared with the return-to-activity rate for nonpitchers, encompassing return to work and return to sport, was 57.5% (84/146 patients) and 87.1% (572/657 patients), respectively, after arthroscopic SLAP repair.
Conclusion: “Arthroscopic SLAP repair is associated with a fair return to sport, with 69.6% of individuals undergoing arthroscopic SLAP repair returning to sport. SLAP repair in pitchers has significantly decreased return to sport in comparison with nonpitching athletes. Athletes on average return to sport within 9 months postoperatively.”
The more surgery, the worse the outcome.
The surgical treatment of SLAP tears continues to be challenging for both the physician and the patient. Of course it becomes much more challenging to the patient if the surgery does not work to the patient’s expectations. Here is a recent paper discussing these problems from doctors at the University of Minnesota and Saarland University in Germany.
- Tears of the superior labrum involving the biceps anchor are a common entity, especially in athletes, and may highly impair shoulder function. If conservative treatment fails, successful arthroscopic repair of symptomatic SLAP lesions has been described in the literature particularly for young athletes.
- However, the results in throwing athletes are less successful with a significant amount of patients who will not regain their pre-injury level of performance (see below for further documentation).
- The clinical results of SLAP repairs in middle-aged and older patients are mixed, with worse results and higher revision rates as compared to younger patients. In this population, tenotomy or tenodesis of the biceps tendon (doctors will move the bicep tendon attachment to a different place on the bone – usually part of a more major surgery) is a viable alternative to SLAP repairs in order to improve clinical outcomes. (6)
Revision surgery for the failed SLAP tear surgery
A study from July 2018 in the The open orthopaedics journal (7) throws a lot of questions at the effectiveness of SLAP tear surgery.
- “Optimal treatment of type II superior labrum anterior and posterior (SLAP) tears is controversial. There has been a recent trend towards biceps tenodesis over SLAP repair in older patients. Few surgeons have performed combined biceps tenodesis and SLAP repair with inferior results.”
- “Failed SLAP repair is often multifactorial and a thorough workup is needed. Combined biceps tenodesis and SLAP repair can cause pain, stiffness, and dysfunction which can be successfully treated with arthroscopic superior capsular release.”
SLAP tear surgery does cause a lot of damage, this is why revision surgery is generally not successful.
Similar findings were observed by surgeons at New York University Hospital for Joint Diseases. They found that on average 10% of patients would need a second shoulder surgery at average two years after the initial SLAP lesion procedure and those procedures were expanded to include subacromial decompression (35%), debridement (26.7%). repeat SLAP repair (19.7%), and biceps tenodesis or tenotomy (13.0%). After isolated SLAP repair, patients aged 20 years or younger were more likely to undergo arthroscopic Bankart repair.
The doctors concluded: “We identified a 10.1% incidence of subsequent surgery after isolated SLAP repair, often related to an additional diagnosis, suggesting that clinicians should consider other potential causes of shoulder pain when considering surgery for patients with SLAP lesions. In addition, the number of isolated SLAP repairs performed has decreased over time, and management of failed SLAP repair has shifted toward biceps tenodesis or tenotomy over revision SLAP repair in more recent years.(8)
Also in the July 2018 edition of The open orthopaedics journal, (9) is another study that suggests that for many patients, SLAP tear surgery is not ideal. Risk factors for failure of SLAP repair include age, smoking, obesity, being female and concomitant bicep pathology(weakened, injured biceps). The researchers of this study cited a previous study that found that once a patient has failed first time repair, 71% will fail conservative therapy and 32% will continue to have suboptimal outcomes after a second surgical intervention.
Doctors say no to surgery that athletes want
Is shoulder surgery the only answer for the athlete who wants a quick return to their sport? To many athletes the answer is yes because the alternative recommendations from their orthopedic specialist of ice, rest, physical therapy and wait six months is not the option they want.
Doctors at Houston Methodist Hospital however made this recommendation in published research in the American Journal of Sports Medicine, “Nonsurgical treatment should be considered for professional baseball players with documented SLAP lesions, as it can lead to acceptable RTP (Return-to-play) and RPP (return to prior performance (before injury)) rates.”(10)
For many, many years before these studies, patients came into the office and would tell us about their shoulder labrum tear and the surgery they had, and the pain they still suffer from, and their desperation not to have another surgery. After talking with the patient we discover that a torn labrum showed up on an MRI, the surgery was performed, but, the pain never went away. Something else was causing the pain. As suggested above in why the surgery fails at higher rate and secondary revision is equally prone to failure is that patient may not even have a Slap tear.
SLAP (labral) lesions may actually be rare injuries
Recently when Stephen C. Weber, MD presented the findings of his study that American Board of Orthopaedic Surgery (ABOS) Part II candidates (young surgeons) may be performing superior labral tear anterior to posterior (SLAP) repairs at greater rates than they should, he noted that the increase in surgeries were leading to poor outcomes and increased complication rates.
One of the reasons too many surgeries were being performed was because MRI suggested a SLAP tear when Slap tears were not there. Dr. Weber noted that magnetic resonance imaging (MRI) scans often produce false positives and that SLAP lesions are difficult to diagnose clinically. Numerous studies suggest that even experts disagree on how to define a type II SLAP tear.
“Furthermore, repairing SLAPs is not a benign process, and caring for failed SLAPs can be very difficult,” said Dr. Weber. “Complications include stiffness, persistent rotator cuff tears next to the portals, and damage to the articular cartilage.”
A recent study published in The open orthopaedics journal(11) discussed the controversies surrounding the treatment of SLAP tears.
“(SLAP tears) are a cause of significant shoulder pain and disability. Management for these (tears are) not standardized. There are no clear guidelines for surgical versus non-surgical treatment, and if surgery is pursued there are controversies regarding SLAP repair versus biceps tenotomy/tenodesis.
“The management of SLAP lesions can be divided into 4 broad categories:
(1) nonoperative management that includes scapular exercise, restoration of balanced musculature, and that would be expected to provide symptom relief in 2/3 of all patients;
(2) patients with a clear traumatic episode and symptoms of instability that should undergo SLAP repair without (age < 40) or with (age > 40) biceps tenotomy or tenodesis;
(3) patients with etiology of overuse without instability symptoms should be managed by biceps tenotomy or tenodesis; and
(4) throwing athletes that should be in their own category and preferentially managed with rigorous physical therapy centered on hip, core, and scapular exercise in addition to restoration of shoulder motion and rotator cuff balance.
Peel-back SLAP repair, Posterior Inferior Glenohumeral Ligament (PIGHL) release, and treatment of the partial infraspinatus tear with debridement, PRP, or (rarely) repair should be reserved for those who fail this rehabilitation program.”
To treat a SLAP tear, you must treat the whole shoulder
SLAP lesions do not happen overnight unless you take a fall with your arm extended. Then you can have an acute tear. More typically SLAP lesions occur as the result of repetitive motion or wear and tear injury. SLAP lesions, therefore, do not happen in isolation, they happen as part of a degenerative shoulder disease problem. People who email me typically describe that they have a SLAP tear as well as a torn tendon, torn rotator cuff muscles, and chronic shoulder instability, sometimes with dislocation. The have all the symptoms of a shoulder that is in a downward spiral: Pain and a lot of noise, clicking, grinding, and popping. They have limited range of motion and a significant decrease in strength. It is for these reasons that shoulder surgery for SLAP tears and lesions is not effective. The surgery does not address the whole shoulder problem.
Regenerative injection therapy, bone marrow derived stem cell injections and Platelet Rich Plasma Therapy injections can accelerate the body’s own inflammatory response to repair the labral damage. But treating the whole shoulder capsule, we can not only repair the labrum, but we can also protect it from damage and shoulder instability caused by compromised shoulder structures, such as ligaments and tendons. By treating the whole shoulder, we can strengthen these weakened elements and stabilize the entire joint.
Platelet Rich Plasma Therapy or PRP is derived from your own blood. The idea behind this treatment is that your blood contains a combination of healing growth factors and blood platelets. To “make” platelet-rich plasma therapy, a small blood draw, similar to the amount taken for blood work is taken from you. The blood is then spun in a centrifuge to separates the platelets from the other components. The concentrated platelet-rich plasma is then injected into and around shoulder.
There is not much published research on stem cell therapy or PRP therapy for tears of the shoulder labrum. Clinically and empirically we have seen many patients with shoulder labrum tears and have helped many avoid surgery. We have published research on: Treatment of shoulder osteoarthritis and rotator cuff tears with bone marrow concentrate and whole bone marrow injections.
A case review study published in the journal F1000 Research (12) reported on two patients who had treatments. Here is the report:
“Labral tears commonly occur in both the general and sporting population, often leading to significant pain and dysfunction. Patients often engage in progressive rehabilitative programs, and surgical intervention may be required in severe cases. Autologous platelet rich plasma (PRP) injections have been growing in popularity in musculoskeletal medicine as an alternative to corticosteroid injections. This paper looks at the effectiveness of PRP injections in glenoid labral lesions.
Methods: The clinical and radiological findings are presented for two patients who have been treated with autologous PRP into the glenohumeral joint adjacent to the labral tear, in conjunction with a progressive rehabilitative program. Follow up occurred at 18 months and 13 months, respectively.
Results: Both subjects tolerated the PRP injection well with no adverse effects, and were compliant with their rehabilitative programs. On initial presentation, pain on the visual analogue scale (VAS) was 7/10 and 6/10 and at follow up it was reported as 0/10. Both subjects have now returned to normal sporting and work activities.”
Treatment options
Above I outlined the conventional conservative care options for a shoulder labral tear. In my other articles on this website I offer more treatment options and research surrounding the non-surgical treatment of shoulder labrum tears.
Bone Marrow derived stem cell therapy and Platelet Rich Plasma Therapy are injection techniques that can accelerate the body’s own inflammatory response to repair the labral damage. But treating the whole shoulder capsule, we can not only repair the labrum, but we can also protect it from damage and shoulder instability caused by compromised shoulder structures, such as ligaments and tendons. By treating the whole shoulder, we can strengthen these weakened elements and stabilize the entire joint.
There is not much research currently on the use of PRP or stem cell therapy for SLAP tears beyond empirically evidence and clinical observation.
A December 2018 study (13) suggested that PRP seemed to work in non-surgical and surgical settings but the definitive medical research is not there yet. This is what that study said:
“The use of PRP in orthopedic surgery is becoming more common, with increasing use in the shoulder in both operative and non-operative settings. . .PRP is thought to promote healing and stimulate growth by the release of growth factors from a high concentration of activated platelets. Yet despite this exciting promise, human subject research with PRP has not produced consistent results in favor of its use in either operative or non-operative conditions of the shoulder, and thus, no consensus exists regarding its therapeutic guidelines or application.
There are some limitations in the study of the efficacy of PRP for the treatment of shoulder pathology. One limitation includes the lack of standardized dosing, formulation, and concentration of the platelets and growth factors that comprise PRP. . . The application of PRP can also differ between administering clinicians, as there is no standardized technique. These variations make cross-study comparisons difficult to interpret.
Based on our review of the current literature, evidence in favor of PRP use for operative and non-operative management of shoulder conditions is inconsistent and cannot be absolutely supported or refuted. The potential benefits of PRP, perhaps not yet (understood), could outweigh the risks, which are minimal.”
References
1 Schrøder CP, Skare Ø, Reikerås O, Mowinckel P, Brox JI. Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial. British Journal of Sports Medicine. 2017;51(24):1759-1766. doi:10.1136/bjsports-2016-097098.
2 Schrøder CP. SLAP lesions, An Opinion Piece. The Open Orthopaedics Journal. 2018;12:342-345. doi:10.2174/1874325001812010342.
3. Johannsen AM, Costouros JG. A Treatment-Based Algorithm for the Management of Type-II SLAP Tears. Open Orthop J. 2018 Jul 31;12:282-287. doi: 10.2174/1874325001812010282. PMID: 30197709; PMCID: PMC6110057.
4 Calcei JG, Boddapati V, Altchek DW, Camp CL, Dines JS. Diagnosis and Treatment of Injuries to the Biceps and Superior Labral Complex in Overhead Athletes. Current Reviews in Musculoskeletal Medicine. 2018:1-9.
5 Chalmers PN, Monson B, Frank RM, Mascarenhas R, Nicholson GP, Bach BR, Verma NN, Cole BJ, Romeo AA. Combined SLAP repair and biceps tenodesis for superior labral anterior–posterior tears. Knee Surgery, Sports Traumatology, Arthroscopy. 2016 Dec 1;24(12):3870-6.
6. Brockmeyer M, Tompkins M, Kohn DM, Lorbach O. SLAP lesions: a treatment algorithm. Knee Surg Sports Traumatol Arthrosc. 2016 Feb;24(2):447-55. doi: 10.1007/s00167-015-3966-0. Epub 2016 Jan 27.
7. Han Y, Lee J, Park S, Suh E. Suppl-1, M5: Superior Capsular Release After Failed Combined Superior Labral Repair And Biceps Tenodesis For Slap Tear. The open orthopaedics journal. 2018;12:295.
8 Mollon B, Mahure SA, Ensor KL, Zuckerman JD, Kwon YW, Rokito AS. Subsequent shoulder surgery after isolated arthroscopic SLAP repair. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016 Oct 31;32(10):1954-62.
9 Charles MD, Christian DR, Cole BJ. Suppl-1, M2: An Age and Activity Algorithm for Treatment of Type II SLAP Tears. The open orthopaedics journal. 2018;12:271.
10 Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to play after treatment of superior labral tears in professional baseball players. Am J Sports Med. 2014 May;42(5):1155-60. doi: 10.1177/0363546514528096. Epub 2014 Mar 27.
11 Hester WA, O’Brien MJ, Heard WM, Savoie FH. Suppl-1, M9: Current Concepts in the Evaluation and Management of Type II Superior Labral Lesions of the Shoulder. The open orthopaedics journal. 2018;12:331.
12 Vander Kraats R, Doss A. Glenoid labral tear: follow up case series on ultrasound guided autologous platelet rich plasma in conjunction with a progressive rehabilitation program. F1000Research. 2012 Dec 19;1.–
13 Lorentz NA, Hurley ET, Colasanti CA, Markus DH, Alaia MJ, Campbell KA, Strauss EJ, Jazrawi LM. Return to Play After Biceps Tenodesis for Isolated SLAP Tears in Overhead Athletes. The American Journal of Sports Medicine. 2022 Mar 28:03635465211041698.
14 LeVasseur MR, Mancini MR, Hawthorne BC, Romeo AA, Calvo E, Mazzocca AD. SLAP tears and return to sport and work: current concepts. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine. 2021 Mar 11.
15 Freijomil N, Peters S, Millay A, Sinda T, Sunset J, Reiman MP. The success of return to sport after superior labrum anterior to posterior (slap) tears: a systematic review and meta-analysis. International Journal of Sports Physical Therapy. 2020 Oct;15(5):659.
16 Thayaparan A, Yu J, Horner NS, Leroux T, Alolabi B, Khan M. Return to sport after arthroscopic superior labral anterior-posterior repair: A systematic review. Sports health. 2019 Nov;11(6):520-7.
17 Sandler AB, Childs BR, Scanaliato JP, Dunn JC, Parnes N. SLAP Repair Versus Biceps Tenodesis in Patients Younger Than 40 Years: A Cost-Effectiveness Analysis. Orthop J Sports Med. 2022 Nov 29;10(11):23259671221140364. doi: 10.1177/23259671221140364. PMID: 36479458; PMCID: PMC9720817.
4263